Cancer Staging
Summary of AJCC 8th Edition Staging Guidelines
- Introduction
- Shared Nodal Categorization & Group Staging
- Oral Cavity
- Oropharynx (p16-)
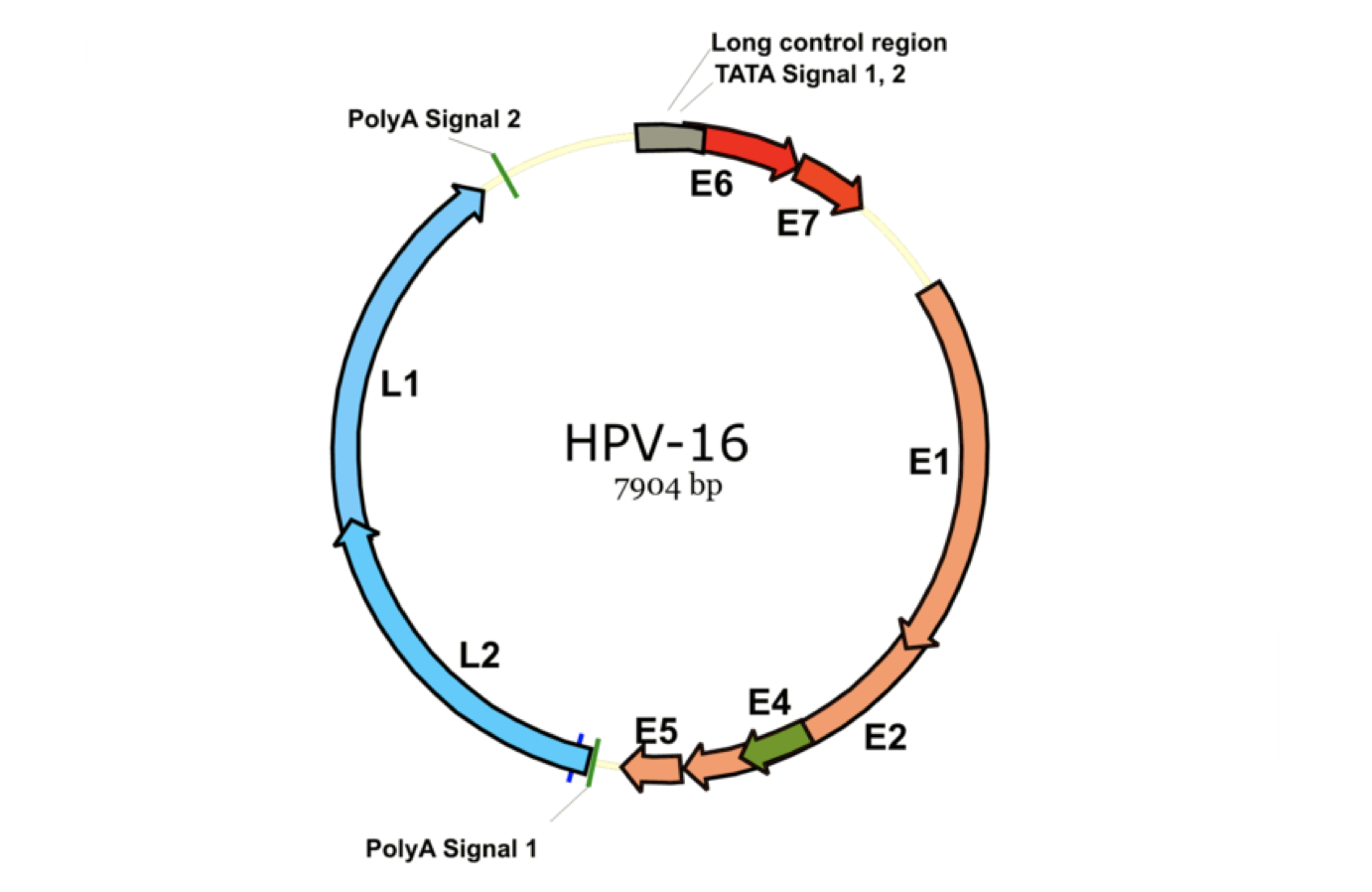
- Oropharynx (p16+)
- Hypopharynx
- Larynx
- Esophagus and Esophagogastric Junction
- Nasal Cavity & Paranasal Sinuses
- Nasopharynx
- Major Salivary Glands
- Sarcomas of the Head & Neck
- Cutaneous Carcinoma of the Head & Neck
- Cutaneous Melanoma
- Mucosal Melanoma of the Head & Neck
- Merkel Cell Carcinoma
- Thyroid (Differentiated)
- Thyroid (Medullary)
- Thyroid (Anaplastic)
- Parathyroid